Inflammation: What It Is, How It Affects Your Body, and What You Can Do
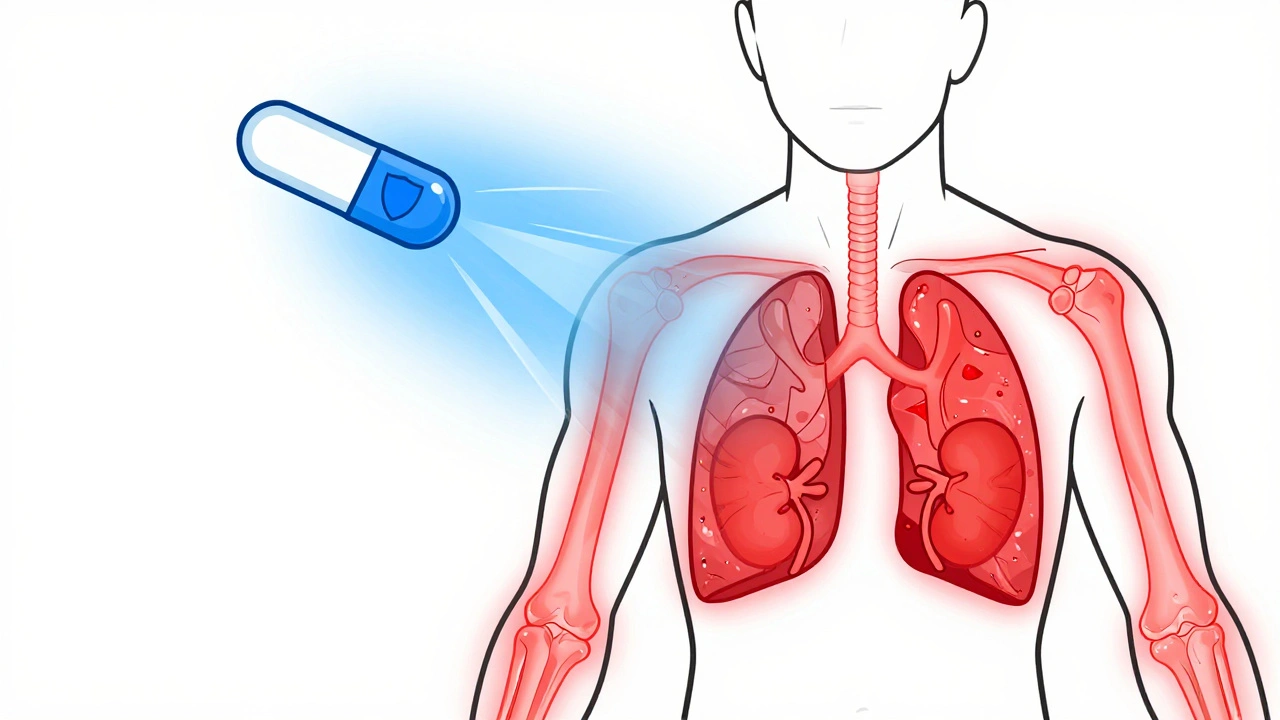
When your body gets hurt or infected, inflammation, the body’s natural defense mechanism to remove harmful stimuli and begin healing. Also known as the immune response, it’s why your skin turns red, swells up, or feels warm after a cut or bug bite. That’s not a problem—it’s working. But when inflammation sticks around too long, it stops being helpful and starts damaging your tissues. That’s called chronic inflammation, a persistent, low-grade immune response linked to conditions like arthritis, heart disease, and diabetes. Unlike the quick, obvious swelling from a sprained ankle, chronic inflammation often creeps up silently, quietly increasing your risk for serious illness.
It’s not just about joints or skin. TNF inhibitors, a class of drugs used to block a key protein that drives inflammation in autoimmune diseases are prescribed because your immune system is overreacting—attacking your own body. Drugs like Humira or Enbrel don’t cure the problem, but they silence the signal telling your body to keep fighting. That’s why they’re used for rheumatoid arthritis, Crohn’s, or psoriasis. But here’s the catch: turning down inflammation too much can leave you vulnerable. That’s why doctors watch for infections or even cancer risk when using these drugs. It’s a balance—reduce the damage without shutting down protection entirely.
Inflammation also plays a role in everyday pain. That backache? The joint stiffness in the morning? Often, it’s not just wear and tear—it’s inflammation hiding in plain sight. That’s why treatments like TENS therapy, a non-drug method that uses electrical pulses to interrupt pain signals can help. It doesn’t reduce inflammation directly, but it breaks the cycle of pain and muscle tension that makes it worse. And when you’re dealing with long-term pain, avoiding opioids becomes even more important. Opioid-induced constipation and neurological side effects are real risks, and they’re often tied to the same chronic inflammation that caused the pain in the first place.
You’ll find posts here that connect the dots between inflammation and medications you might be taking—whether it’s how insulin interacts with inflammation in diabetes, why some generic drugs might not control it as well, or how pregnancy changes how your body handles immune responses. There’s no magic bullet, but understanding inflammation helps you ask the right questions. What’s really causing your pain? Is it temporary, or is your body stuck in fight mode? And what’s the safest way to bring it under control without trading one problem for another?
Corticosteroids for Autoimmune Disease: Benefits and Long-Term Risks
Corticosteroids quickly reduce inflammation in autoimmune diseases like lupus and rheumatoid arthritis, but long-term use carries serious risks including bone loss, cataracts, and adrenal suppression. Learn how to use them safely and what alternatives exist.
read more