Prednisone: What It Is, How It Works, and What You Need to Know
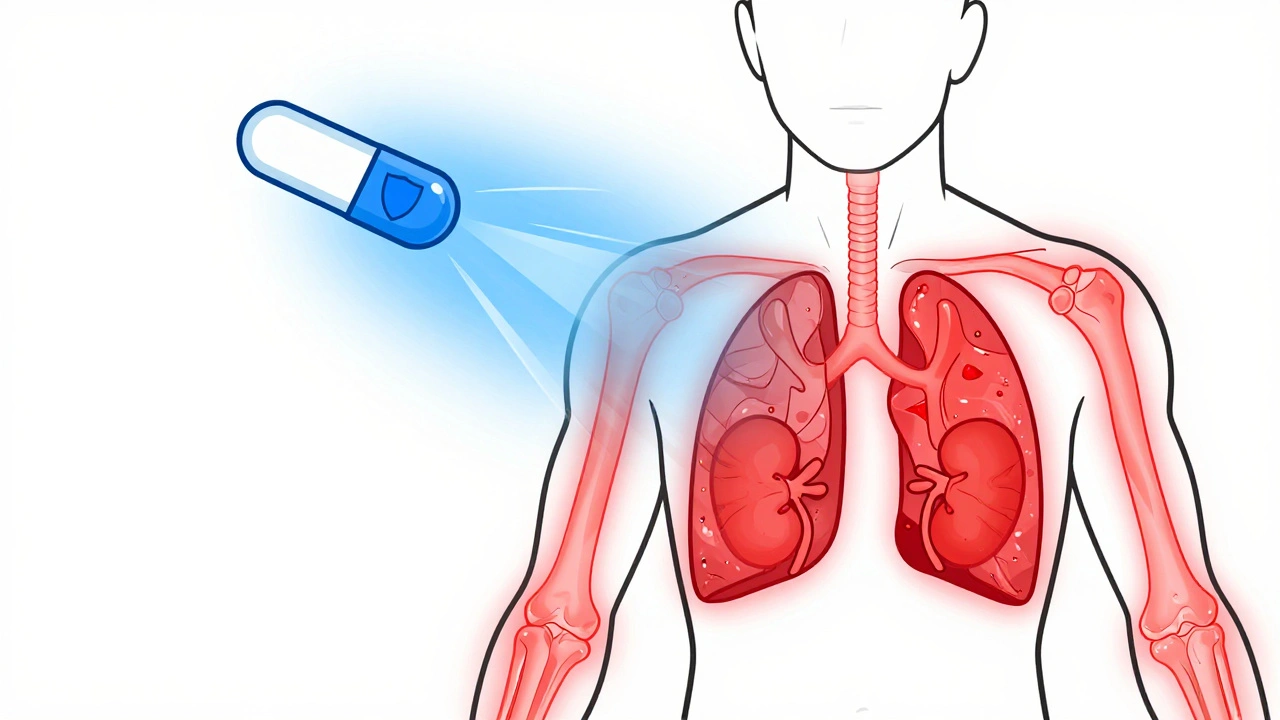
When your body’s immune system goes into overdrive—attacking your joints, lungs, or skin—it’s often prednisone, a synthetic corticosteroid that mimics natural hormones to calm immune responses and reduce swelling. Also known as a corticosteroid, it’s one of the most prescribed drugs for autoimmune conditions, severe allergies, and inflammatory diseases. Unlike painkillers that just mask symptoms, prednisone targets the root cause: unchecked inflammation.
Prednisone doesn’t cure anything. It buys time. It’s the tool doctors reach for when conditions like rheumatoid arthritis, lupus, or severe asthma flare up. But it’s not harmless. Because it suppresses your immune system, you’re more vulnerable to infections. Long-term use can lead to bone thinning, weight gain, high blood sugar, and even mood swings. The key isn’t avoiding it—it’s using it smartly. Many people take it for weeks or months, not years. Others need it for life, but at the lowest possible dose. Your doctor will monitor your blood pressure, blood sugar, and bone density because prednisone doesn’t just affect your immune system—it changes how your body handles sugar, salt, and calcium.
It’s also linked to other medications you might be taking. If you’re on NSAIDs, like ibuprofen or naproxen, used for pain and inflammation, combining them with prednisone raises your risk of stomach ulcers. If you’re on diabetes medication, like insulin or metformin, to control blood sugar, prednisone can make your levels spike—sometimes dramatically. And if you’ve been on prednisone for more than a couple weeks, you can’t just stop it. Your body stops making its own cortisol. Stopping suddenly can trigger adrenal crisis—low blood pressure, vomiting, even collapse. Tapering off slowly isn’t optional; it’s life-saving.
What you’ll find below isn’t a list of every study ever done on prednisone. It’s a collection of real, practical questions people face when taking it. How does it interact with other drugs? What side effects are most common—and which ones mean you need to call your doctor right away? How do you protect your bones, your blood sugar, and your mental health while on it? These posts don’t just explain the science—they show you how to live with it. Whether you’re just starting prednisone or have been on it for years, the articles ahead give you the tools to take control—not just of your condition, but of your treatment.
Corticosteroids for Autoimmune Disease: Benefits and Long-Term Risks
Corticosteroids quickly reduce inflammation in autoimmune diseases like lupus and rheumatoid arthritis, but long-term use carries serious risks including bone loss, cataracts, and adrenal suppression. Learn how to use them safely and what alternatives exist.
read more