Cancer Risk: What Increases It and How to Understand the Real Threats
When we talk about cancer risk, the likelihood of developing cancer over a lifetime due to a mix of genetic, environmental, and behavioral factors. Also known as cancer susceptibility, it’s not a single number—it’s a pattern shaped by what you eat, how you live, and even where you work. Many people assume cancer is mostly bad luck, but research shows up to 40% of cases are linked to preventable causes. That means your daily habits matter more than you think.
Lifestyle factors, choices like smoking, alcohol use, physical activity, and diet play a huge role. Smoking isn’t just linked to lung cancer—it raises risk for at least 15 types, including bladder, throat, and pancreatic. Heavy drinking increases liver and breast cancer risk. Being overweight or inactive adds pressure on your body’s repair systems, making cells more likely to turn cancerous. These aren’t vague warnings—they’re backed by decades of population studies tracking millions of people.
Environmental carcinogens, substances in air, water, or products that directly damage DNA are harder to avoid but still manageable. Think asbestos in old buildings, radon in basements, or even certain chemicals in processed meats. UV radiation from the sun is one of the most common—skin cancer is the most preventable type if you use sunscreen and avoid tanning beds. You don’t need to live in a bubble, but knowing where these hidden dangers hide helps you cut exposure without panic.
Then there’s screening guidelines, structured tests like colonoscopies, mammograms, or HPV tests that catch cancer early when treatment works best. These aren’t optional checkups—they’re proven life-savers. A colonoscopy can remove precancerous polyps before they turn dangerous. A Pap smear finds abnormal cervical cells years before cancer develops. Skipping screenings because you feel fine is like ignoring a check engine light because the car still drives. The goal isn’t to scare you—it’s to give you control.
What you won’t find here are miracle cures or fear-based claims. The posts below focus on real, evidence-backed connections: how certain medications affect long-term cancer risk, why some supplements might help or hurt, how chronic inflammation from conditions like GERD or hepatitis leads to tumors, and what blood tests or imaging can actually tell you about your status. You’ll see how opioid use ties to immune changes, how corticosteroids alter cell behavior, and why managing diabetes or liver damage matters beyond the obvious symptoms.
This isn’t about guessing whether you’ll get cancer. It’s about understanding what parts of the puzzle you can actually change—and what parts you should monitor. The goal is clarity, not confusion. You don’t need to eliminate every possible risk. You just need to know which ones matter most, and how to act on them without losing sleep over the rest.
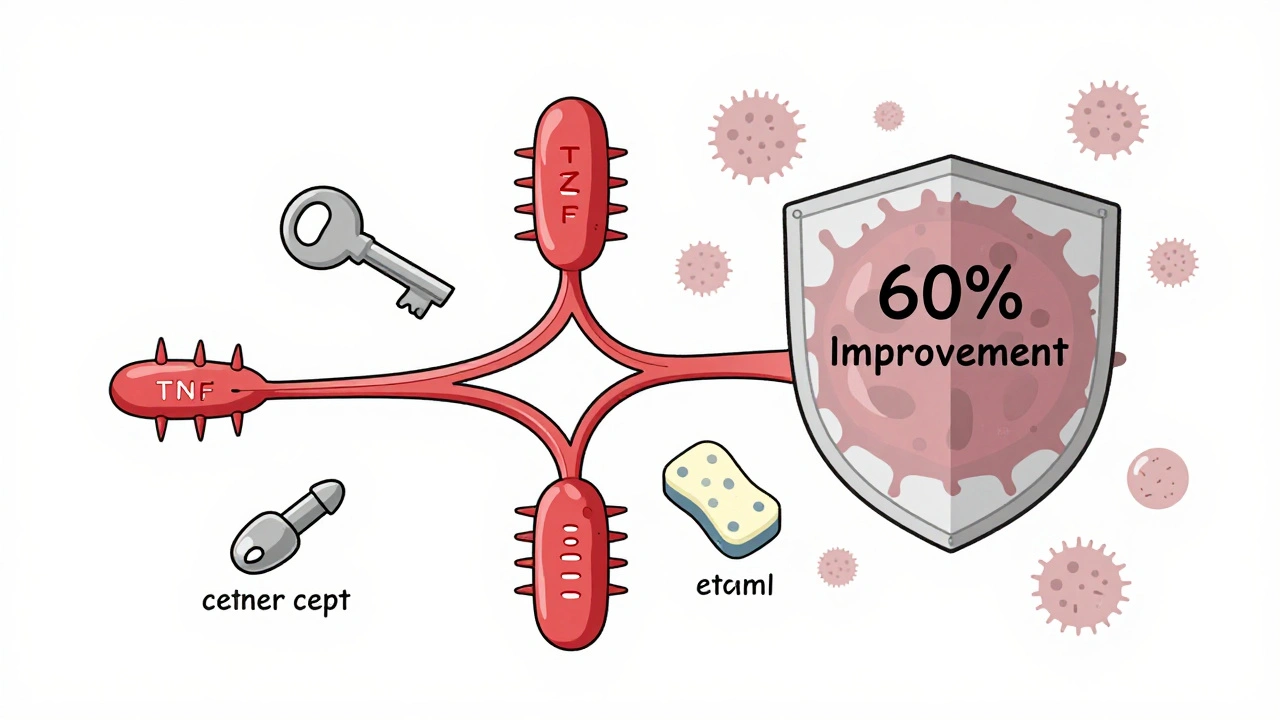
TNF Inhibitors and Cancer Risk: What You Need to Know About Biologics and Immunosuppression
TNF inhibitors like Humira and Enbrel are powerful treatments for autoimmune diseases, but concerns about cancer risk persist. Latest studies show no overall increase in cancer risk, with important differences between drugs and personal risk factors that guide safe use.
read more